Bee Sting Serum Sickness
Bee venom, a complex mixture of proteins and peptides, is known for its ability to provoke a range of reactions in the human body. Ranging from minor local inflammation to severe systemic responses, these reactions can include an uncommon but significant condition known as serum sickness. This phenomenon occurs when the immune system overreacts to certain substances introduced into the body, like bee venom or certain medications and vaccines. How to handle bee sting serum sickness?
Serum sickness represents a type I hypersensitivity reaction typically characterized by symptoms such as fever, rash, joint pain, and swelling appearing one to two weeks after exposure. Understanding this condition entails detailed knowledge about immunological processes, diagnostic procedures, and available treatment options. It also requires sensitivity towards susceptible individuals who may be at risk due to their inherent drive towards service professions involving interactions with nature or outdoor environments. By broadening awareness about bee sting serum sickness, it becomes possible to equip these individuals with preventive measures and timely interventions. Furthermore, antibiotics and injections can cure armpit pain after a bee sting.
Understanding Bee Venom
Bee venom, a complex mixture of proteins and peptides, is critical in triggering serum sickness when an individual is stung. This venom composition varies among different bee species but generally contains enzymes, biogenic amines, lipids, and other bioactive components. The primary active constituents are proteins like melittin and apamin, which induce various physiological reactions. Interestingly, allergenic proteins such as phospholipase A2 (PLA2) and hyaluronidase within the venom are chiefly responsible for allergic reactions.
The mechanism behind allergic reactions to bee stings involves the immune system’s response to these allergenic proteins. Upon first exposure to bee venom, certain individuals may become sensitized; their immune systems recognize the allergens as threats and produce specific antibodies called Immunoglobulin E (IgE). If another sting occurs later on from the same or similar species of bees, these IgE antibodies bind to the venom’s allergens. This binding leads to a cascade of biochemical events that ultimately result in allergic symptoms ranging from local inflammation to systemic anaphylaxis.
Understanding bee venom has significant implications for medical research and treatment development despite its potential dangers. The intricate interplay between its components provides insights into pathophysiological processes related to inflammatory responses and immune modulation. Subsequently, this paved the way for innovative therapeutic strategies targeting diseases characterized by abnormal immune responses, such as allergies or autoimmune disorders.
Thus providing an unexpected silver lining even while dealing with something potentially harmful like bee stings. With this foundational knowledge about what constitutes bee venom and how it interacts with our bodies, we can now delve deeper into exploring what exactly serum sickness is all about.
What is Serum Sickness
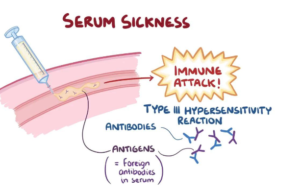
Characterized by a constellation of symptoms such as rash, fever, and joint pain, this immune response typically occurs after exposure to certain medications or substances. Serum sickness is an example of such an immune response. A delayed hypersensitivity reaction arises following the administration of large amounts of non-human (heterologous) proteins or other antigens into the human body. These foreign proteins trigger the immune system to produce antibodies, forming complexes with the foreign proteins or antigens. The deposition of these immune complexes in various tissues leads to inflammation and damage – a defining characteristic of serum sickness.
The table below provides a visual representation demonstrating the mechanism via which serum sickness occurs:
| Step | Description | Outcome | | —- | ———– | ——- | | 1 | Administration of heterologous protein or antigen into the human body | Immune System Activation | | 2 | Antibodies produced by the Immune System combine with foreign protein/antigen | Formation of Immune Complexes | | 3 | Deposition of Immune Complexes in various tissues | Inflammation and Damage |
Progression through this cascade can lead to several clinical manifestations, including malaise, fever, skin rashes, joint pain, lymphadenopathy (swollen lymph nodes), and splenomegaly (enlarged spleen). It’s essential for healthcare professionals to be aware and vigilant about these signs when treating patients who have been administered treatment involving heterologous proteins – like bee venom therapy, for instance.
Understanding serum sickness helps medical practitioners anticipate potential complications related to treatments involving heterologous proteins. This knowledge assists them in making informed decisions while administering care that best serves their patient’s health needs. As we delve further into our discussion on ‘bee sting serum sickness’, it becomes clear that recognizing the symptoms associated with this condition is crucial for timely diagnosis and treatment management. Many people want to know about can a bee sting cause swollen lymph nodes?
Symptoms of Bee Sting Serum Sickness
Symptoms associated with an adverse reaction to hymenoptera venom therapy, a known heterologous protein, often mirror those seen in serum sickness and may include malaise, fever, skin rashes, joint pain, lymphadenopathy, and splenomegaly. The onset of these symptoms usually occurs one to two weeks after the administration of the allergenic substance and can persist for several days or even weeks. Patients typically describe feeling generally unwell during this period, with fatigue being a commonly reported symptom. Fever may accompany the general malaise and is often indicative of an ongoing immune response. Skin manifestations are quite common, ranging from mild urticaria to more severe eruptions resembling erythema multiforme.
Sickness progression varies among individuals based on factors such as the amount of venom introduced into the body through the sting, individual sensitivity to bee venom proteins, and previous exposure history. Allergic reactions accompanying bee sting serum sickness can be immediate or delayed. Immediate hypersensitivity responses typically manifest within minutes to hours post-sting and involve IgE antibodies while delayed reactions are mediated by IgG or IgM antibodies forming immune complexes that deposit in tissues, causing inflammatory responses leading to symptoms like arthralgia (joint pain), lymph node swelling (lymphadenopathy), enlargement of spleen (splenomegaly), and various skin rashes.
The transition from experiencing symptoms to seeking diagnosis often depends on their severity or persistence beyond expected recovery timescales following a bee sting event. Individuals should remain vigilant for any abnormal signs or changes in their health condition post-exposure since early detection aids in effective treatment planning for bee sting serum sickness. Following a suspicion of this disorder due to observed symptomatic indications, diagnostic methods and medical procedures are employed to confirm its presence, thus facilitating appropriate treatment interventions.
Diagnosis and Medical Procedures
In the realm of medical diagnostics, around 20% of individuals with classic serum sickness-like reactions are found to have demonstrable immune complexes or complement consumption, underscoring the importance of comprehensive testing procedures. The diagnosis process for bee sting serum sickness typically involves a combination of a patient’s clinical history, physical examination findings, and laboratory tests. Laboratory tests primarily include complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level assessments. As part of the diagnostic procedure, Serum Testing Methods like Enzyme-linked immunosorbent assay (ELISA) can be employed to detect specific antibodies that might confirm an allergic reaction to bee venom.
- Physicians may use In Vivo testing methods such as skin prick test or intradermal test for immediate hypersensitivity reactions.
- In Vitro, testing methods such as Radioallergosorbent Test (RAST) can be used when skin tests are contraindicated.
- Complement levels in the blood may also be evaluated since low complement levels could indicate an ongoing immune response due to serum sickness.
Recognizing and diagnosing bee sting serum sickness promptly is crucial in managing the condition effectively and preventing potential Medical Complications such as glomerulonephritis, vasculitis, and arthritis. These complications arise from prolonged exposure to circulating immune complexes depositing into various tissues, leading to inflammation and damage. The severity of these complications underscores the importance of timely diagnosis and intervention.
The process involved in determining whether symptoms align with those typical of bee sting serum sickness is both intricate and exhaustive. However, this meticulous approach is required given that early detection significantly increases positive health outcomes whilst decreasing adverse effects associated with delayed treatment interventions. With a clear understanding of potential risks associated with undiagnosed or untreated cases, it becomes paramount for healthcare professionals to explore all possible avenues during diagnostic processes while maintaining patient comfort throughout. The subsequent section will explore various treatment options to ameliorate bee sting serum sickness and its associated symptoms.
Treatment Options
Managing this type of hypersensitivity reaction involves a multifaceted treatment approach, including immediate interventions, pharmacological therapy, and preventive strategies. If a bee sting leads to serum sickness, medical professionals may initially remove the stinger if it is still present and apply a cold pack to alleviate swelling and discomfort. Steroids are often administered orally or intravenously to suppress the immune system’s overreaction. In severe cases where there is difficulty breathing due to throat swelling, an adrenaline injection may be necessary.
Pharmacological therapies include antihistamines, which can help manage symptoms such as itching, rashes, and hives caused by the release of histamines in response to the allergen. As part of a holistic treatment plan, natural antidotes like honey or apple cider vinegar might be used for their anti-inflammatory properties. Home remedies can also effectively manage milder symptoms; baking soda mixed with water forms a paste that can soothe irritation when applied topically, while herbal teas containing nettle or chamomile have been known to relieve systemic allergic reactions.
Although treating acute manifestations of serum sickness from bee stings is essential, focusing on long-term management and preventive measures is equally important. Immunotherapy or desensitization therapy is an option for patients who experience repeated episodes of severe allergy from bee stings. This involves gradually increasing doses of venom injections over time so that the immune system becomes less reactive to it. It is crucial that individuals understand these treatment options along with recognizing early signs of serum sickness for timely intervention and minimizing complications. The next section will further detail these preventative measures without resorting to step-by-step instructions.
Preventive Measures
Preventive measures play a crucial role in mitigating the risk of hypersensitivity reactions, particularly for individuals with known allergies. The most effective way to prevent bee sting serum sickness is to avoid getting stung by bees. This may involve being cautious in environments where bees are commonly found, such as gardens, orchards, and forests. Wearing protective clothing and avoiding strong fragrances that might attract bees can also be beneficial. Allergy vaccinations or immunotherapy represent another key preventive measure against bee sting serum sickness for those at high risk.
Apart from Sting Avoidance and Allergy Vaccinations, some additional preventive measures include: – Continuous monitoring: For individuals who have experienced a severe reaction to a bee sting in the past, carrying an emergency epinephrine autoinjector (EpiPen) can be lifesaving. – Prevention education: Understanding how to react when encountering bees can prevent panic-induced actions that might provoke an attack. – Medical Alert Jewelry: Wearing medical identification jewelry indicating one’s allergy status can aid swift treatment provision during emergencies. – Regular check-ups: Routine medical follow-ups help monitor any changes in one’s allergic response over time. – Safe recreational planning: Planning outdoor activities outside peak bee activity periods or avoiding areas with high bee populations.
Without resorting to summation phrases, it must be underscored that prevention is indeed better than cure when dealing with potential hypersensitivity reactions like bee sting serum sickness. One cannot underestimate the importance of understanding these preventive measures and implementing them consistently, especially if they are at increased risk due to previous severe allergic reactions or known sensitivities. It’s not just about personal well-being but also contributing towards a collective effort in reducing healthcare burdens associated with allergic conditions. By adopting these strategies – from simple behavioral modifications like sting avoidance techniques to more advanced interventions like allergy vaccinations – individuals become proactive participants in their own health journey while also serving others by setting an example of responsible health practice.
Frequently Asked Questions
Is bee sting serum sickness contagious?
Serum sickness, including that triggered by bee stings, is not contagious. Preventive measures focus on avoiding allergens and managing serum reactions promptly to mitigate potential complications. Public health education plays a critical role in prevention.
Can bee sting serum sickness reoccur after successful treatment?
In approximately 15% of patients, Serum Sickness can reoccur even after successful treatment. Prevention includes Allergy Immunotherapy, which helps the body build tolerance to allergens such as bee venom, thereby reducing recurrence chances.
Are there any long-term effects or complications associated with bee sting serum sickness?
Serum sickness prognosis generally indicates no long-term effects or complications. However, the immunological mechanisms involved can occasionally lead to recurrent symptoms if re-exposed to the same allergen, warranting careful future avoidance strategies.
Can certain diets or lifestyle changes help in managing bee sting serum sickness?
Evidence shows that specific diets or lifestyle alterations do not directly influence serum sickness prevention. However, allergen desensitization protocols can be beneficial in managing the immune response to bee sting venom.
Are there any alternative or holistic treatments for bee sting serum sickness?
Homeopathic remedies and herbal interventions, such as calendula or echinacea, may provide relief for serum sickness symptoms. However, these treatments should complement, not replace, medical advice and conventional therapeutic approaches.
Conclusion
In conclusion, the phenomenon of bee sting serum sickness is akin to a delicate dance between venom and immune response, with potentially harmful consequences. Learn more about Is a bee sting in the neck dangerous. Understanding its mechanisms, symptoms, and treatments offers valuable insights into managing this immunological ballet. Preyon Pest Control is reliable in controlling any type of pests. Contact them at 708-232-7703.
Efforts towards preventing bee stings can reduce instances of serum sickness. Furthermore, improvements in medical diagnostics and treatments may enhance patient outcomes. In essence, navigating the intricacies of bee sting serum sickness requires a blend of vigilance, scientific understanding, and medical intervention.